 |
 |
AbstractBackground and ObjectivesFibrin sealant (FS) is widely used to reduce postoperative bleeding. This analysis aimed to assess the efficacy of FS to reduce complications after rhinoplasty.
Materials and MethodWe searched PubMed, Scopus, Embase, the Cochrane Library, and the Web of Science database for articles on FS and rhinoplasty from the inception of publication to December 29, 2021. Post-rhinoplasty complications, such as edema and ecchymosis, were recorded. The final meta-analysis was performed using three studies.
ResultsTwo subgroups were created based on the FS usage after rhinoplasty. The FS effect on edema reduction was favorable on the postoperative day-1 (standardized mean difference [SMD]=-1.07 [-1.70; -0.45]). In addition, the FS effect on ecchymosis reduction was favorable on the postoperative day-1 postoperative (SMD=-1.33 [-2.15; -0.50]).
IntroductionAccording to the American Society of Plastic Surgeons cohort study, facial plastic surgery is steadily increasing with the growth of the gross domestic product [1]. In particular, the rhinoplasty rate is second only to the rate of minimally invasive cosmetic surgeries [1]. Although rhinoplasty is considered a cosmetic surgery, complications such as edema and ecchymosis frequently occur after the procedure. Such complications aggravate patient discomfort and delay a return to daily life. Consequently, various therapeutic methods such as steroids, intraoperative hypotension, intraoperative cooling, head elevation, piezosurgery, and tranexamic acid have been tested to reduce morbidities after rhinoplasty [2-5]. Some of these treatments are known to reduce postoperative morbidities, but some remain controversial [4]. Despite considerable effort, edema and ecchymosis are still frequent after rhinoplasty, and are a major cause of deterioration in patient quality of life. Moreover, severe edema and ecchymosis can increase scarring and alter intended surgical outcomes [6,7].
Surgical method characteristics can also affect postoperative morbidities. The surgical techniques used in rhinoplasty are classified into open (external) rhinoplasty and closed (endonasal) rhinoplasty [8]. Endonasal rhinoplasty is associated with low morbidities and results in a natural appearance. This outcome is achieved by retaining the original shape of the nose and preserving major cartilage architectures. However, endonasal rhinoplasty has disadvantages as it is a difficult surgical technique, provides limited visibility, and allows inadequate accessibility to cartilage. On the other hand, open rhinoplasty is a more straightforward method for accessing cartilage, and is preferred for highly complex surgeries and educational purposes. However, open rhinoplasty also has disadvantages including a high complication rate and delayed recovery time. High postoperative morbidities might be expected because soft tissue bleeding is inevitable due to the nature of external rhinoplasty. In particular, it is known that osteotomy, which is frequently performed in rhinoplasty, increases morbidities such as edema and ecchymosis [9]. Because open rhinoplasty and osteotomy cannot be completely avoided, methods to reduce postoperative morbidities more effectively are needed.
Fibrin sealant (FS) is a plasma cryoprecipitate-based sealant that consists of two components: human sealer protein and human thrombin [10]. The invention of this sealant was based on the development of the fibrin network that represents the final phase in the blood coagulation process. Morawitz [11] was the first to describe the physiological mechanism of FS. Since it was invented, FS has been widely used for suture support, tissue adhesion, and hemostasis. Several studies have shown that FS reduces postoperative bleeding and ecchymosis by sealing capillary vessels, which in turn lessens postoperative swelling by promoting wound adhesion and minimizing dead space [12,13]. Recently, attempts were made to test the efficacy of FS to reduce postoperative complications after rhinoplasty. Consequently, the purpose of this meta-analysis was to investigate whether the application of FS could reduce the severity of complications such as edema and ecchymosis after rhinoplasty. We reviewed randomized controlled trials (RCTs) that compared the rate of complications after rhinoplasty between patients who were treated with FS, and those who were not.
Materials and MethodsProtocol and registrationThis study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [14].
Selection criteriaOnly RCTs comparing patients (≥18 years) who underwent open rhinoplasty with or without osteotomy, and with or without FS treatment were included in this review. The outcomes of interest were postoperative edema (swelling) and ecchymosis (bruising) of the nose and eyes.
Search strategyPubMed, Scopus, Embase, The Cochrane Library, and Web of Science databases were searched to retrieve indexed articles for this study. Articles published in languages other than English were excluded. The final search was conducted on December 29, 2021. The basic search expressions were as follows: (rhinoplasty OR osteotomy) AND (fibrin OR fibrin glue OR fibrin sealant) AND (edema OR swelling OR bruise OR ecchymosis) AND randomized controlled trial. We also considered alternative spellings and abbreviations in the database search process. Relevant reviews were also manually searched and assessed to identify any dropped articles in the search process.
Data extraction and quality assessmentThe full article texts were independently evaluated twice for eligibility by review authors. Disagreements were resolved by consensus through discussion among the authors, JWK and KHL. The collected data were as follows: first author’s name, publication year, study design, number of patients, mean age of the patients, type of control group, osteotomy conduction, type of FS, time of follow-up, and outcomes. The bias and quality of the RCTs were assessed using RevMan 5, which is a Cochrane Collaboration tool. The domains of assessment were as follows: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases. The domains were rated by three grades: high risk, low risk, and unclear risk of bias.
Measures of postoperative outcomeSince heterogeneity exists in meta-analyses of postoperative outcome data, a random effects model was used for meta-analysis with data from the included RCTs. The relative risks for assessment scales of postoperative outcomes were calculated as the standard mean differences. Ninety-five percent confidence intervals were used for statistical significance. Statistical analyses were conducted using R software (version 4.1.0) with the meta and metaphor packages.
ResultsStudy selection and characteristicsA total of 26 studies were retrieved using the search expressions to query the five databases (Fig. 1), and 16 duplicates were subsequently excluded. Detailed numbers of studies at each stage are described in the PRISMA flowchart (Fig. 1). Five studies were excluded after screening the titles and abstracts. Two studies were excluded from the eligibility process due to the absence of appropriate outcome data. Finally, the three remaining eligible studies were analyzed in this meta-analysis study [13,15,16].
Study characteristicsThe characteristics of the included studies are presented in Table 1. The total number of subjects in all the studies was 60, with a mean age of 35.1 years. In the study by Pryor, et al. [13], 10 participants underwent application of FS on one side and not on the contralateral side, and the postoperative complications were compared between the two sides. In another study by Yu, et al. [15], 41 participants underwent rhinoplasty without osteotomy in Korea. In other studies, 19 participants underwent rhinoplasty in the United States. All the studies measured edema and ecchymosis of the nose and eyelid on day-1 and at 1-week postoperatively. A five-level grading scale was used for the 41 participants in the Yu, et al. [15] study. Two other studies applied a 10 cm visual analog scale to evaluate the severity of postoperative edema and ecchymosis complications.
Risk of bias within studiesThe quality of the three studies was assessed using Rev-Man 5, which is recommended by the Cochrane Collaboration to determine risk of bias. A summary of the assessment is presented in Fig. 2. Participant blindness was generally maintained because patients could not know whether FS was applied or not. However, selection and detection bias could not be fully assessed in the first two studies shown in Fig. 2 due to a lack of detailed descriptions. We found considerable variation in the quality of the included studies, which ranged from low to good quality (Fig. 2). One of the three RCTs (Yu, et al. [15] has good reliability, while the other (Dayan, et al. [16]) has high bias, low reliability, and a small sample size. Hence, the findings of Yu, et al. [15] and Pryor, et al. [13] more influence the conclusions of this study than that of Dayan, et al. [16]
Postoperative edema
Fig. 3 shows a forest plot for edema severity with or without FS application on day-1 and at 1-week postoperative. A heterogeneity analysis revealed I2 values of 25% (p=0.26) on day-1 and 0% (p=0.66) at 1-week postoperative, indicating no significant heterogeneity. On day-1 postoperative, two studies showed reduced edema severity after FS application (Pryor, et al. [13], standardized mean difference [SMD]=-1.11 [-2.07; -0.15], Yu, et al. [15], SMD=-1.40 [-2.09; -0.71]). At 1-week postoperative, all studies failed to show any FS effectiveness. The overall pooled effect of FS in reducing edema was favorable only on day-1 postoperative (SMD=-1.07 [-1.70; -0.45]), and not at 1-week postoperative (SMD=-0.40 [-0.88; 0.07]).
Postoperative ecchymosisSimilar to Figs. 3 and 4 shows the severity of ecchymosis with or without FS application on day-1 and at 1-week postoperative. A heterogeneity analysis of ecchymosis severity revealed I2 values of 48% (p=0.15) on day-1 and 75% (p=0.02) at 1-week postoperative. On day-1 postoperative, two studies showed reduced ecchymosis severity after FS application (Pryor, et al. [13], SMD=-2.24 [-3.41; -1.07], Yu, et al. [15], SMD=-1.18 [-1.85; -0.51]). At 1-week postoperative, only one study showed favorable outcomes after FS application (Pryor, et al. [13], SMD=-1.31 [-2.30; -0.32]). The overall pooled effect for FS reduction of ecchymosis was also favorable only on day-1 (SMD=-1.33 [-2.15; -0.50]), and not at 1-week (SMD=-0.16 [-1.28; 0.95]) postoperative.
DiscussionVarious studies have attempted to identify the benefits and side effects of FS application in otolaryngology. A previous study of 100 parotidectomy patients confirmed that application of FS caused very few side effects [17]. Another report showed that FS could replace drainage in thyroidectomy [18,19]. Other surgical uses for FS include reduction of the transfusion rate in femoral neck fractures and knee surgeries [20,21]. An additional study confirmed that FS reduced the risk of leakage in laparoscopic common bile duct incision [22].
Postoperative edema and ecchymosis are the most common side effects of rhinoplasty. Meticulous techniques and standard hemostasis are crucial and cannot be replaced by hemostatics. However, the surgical field of rhinoplasty is very narrow and commonly involves soft tissue and bony destruction. These features allow surgeons performing rhinoplasty to use an applicable hemostatic method. The main purpose of this study was to evaluate whether FS could reduce complications frequently occurring in patients who undergo rhinoplasty. We analyzed three RCTs that studied the effects of FS on the rate of postoperative complications.
The adhesive, sealing, and hemostatic properties of FS may be useful in rhinoplasty. FS can reduce capillary bleeding and serous exudate at the operative site. Two of the three studies included in this meta-analysis demonstrated an advantage associated with FS application on day-1 after rhinoplasty. An FS effect on the reduction of complications was observed only during the initial few days after surgery and not at 1-week postoperative. This outcome could be due to the gradual recovery over time of patients without FS application. The results from this study showed that the application of FS reduced early capillary bleeding and exudate. Considering that patient discomfort is severe in the initial period just after surgery, we expect that the use of FS will be acceptable. An additional advantage for patients is a possible early return to daily life and work. Furthermore, it is encouraging that the three studies analyzed in this meta-analysis did not report any serious side effects, such as allergic reactions to FS.
Our study has several limitations. First, the number of papers and participants in this meta-analysis is small, and the sample size is skewed toward a single paper. Second, the three RCTs have distinct designs, and some of them deviate slightly from the RCT standard. Thus, interpretation requires prudence. However, to the best of our knowledge, this is the first meta-analysis to assess the effects of FS in preventing rhinoplasty-associated morbidities, including ecchymosis and edema.
In conclusion, FS significantly reduced 1-day postoperative complications such as ecchymosis and edema in patients who underwent rhinoplasty. Further large-scale studies on the efficacy of FS to reduce surgical complications after rhinoplasty are needed.
NotesAuthor Contribution Conceptualization: Kun Hee Lee. Data curation: Jeong Wook Kang, Je Ho Bang. Formal analysis: Jeong Wook Kang. Investigation: Jeong Wook Kang, Je Ho Bang. Methodology: Kun Hee Lee. Project administration: Jeong Wook Kang, Seung Yup Son. Supervision: Kun Hee Lee. Writing—original draft: Jeong Wook Kang, Kun Hee Lee. Writing—review & editing: Jeong Wook Kang, Je Ho Bang, Kun Hee Lee. Fig. 2.Risk of bias assessment. A: Risk of bias and applicability concerns graph. B: Risk of bias and applicability concerns summary. 
Fig. 3.Forest plot of edema after rhinoplasty with or without FS application. A: Edema on day-1 after rhinoplasty. B: Edema 1 week after rhinoplasty. SD, standard deviation; SMD, standardized mean difference; CI, confidence interval. 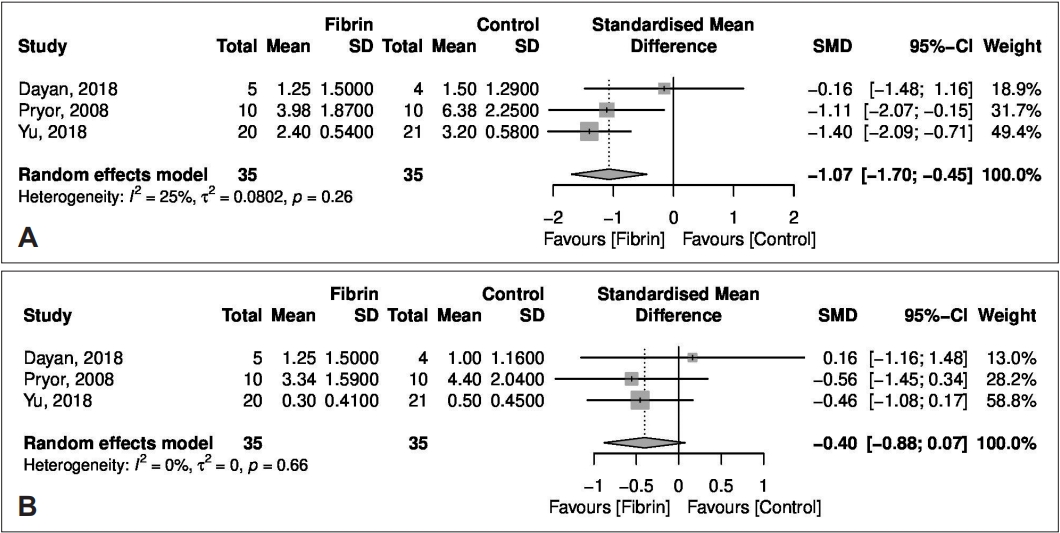
Fig. 4.Forest plot of ecchymosis after rhinoplasty with or without FS application. A: Ecchymosis on day-1 after rhinoplasty. B: Ecchymosis 1 week after rhinoplasty. SD, standard deviation; SMD,standardized mean difference; CI, confidence interval. 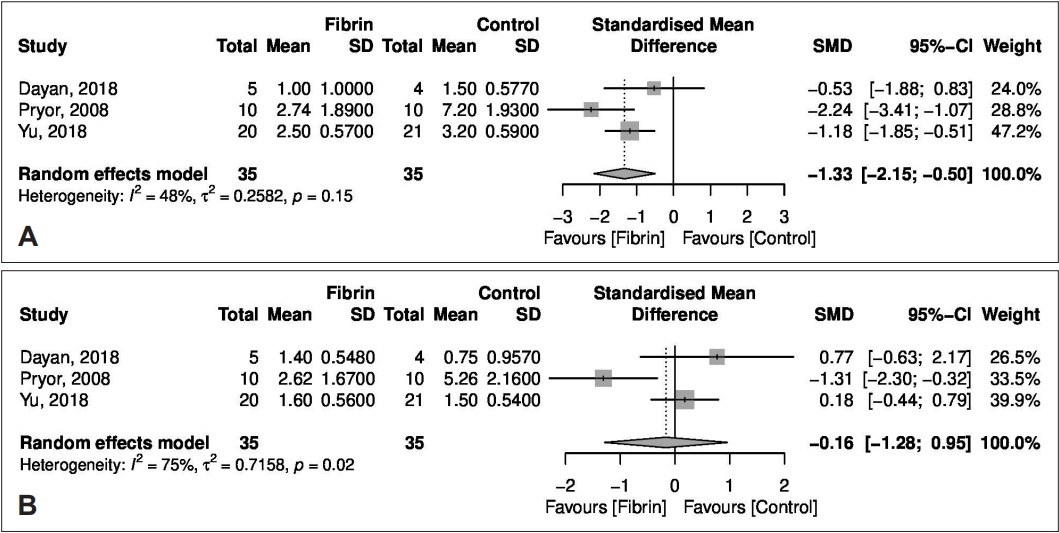
Table 1.Summary of studies included in the meta-analysis
REFERENCES1. Gadkaree SK, McCarty JC, Weitzman RE, Derakhshan A, Mohan S, Bergmark RW, et al. Associations between national financial trends and facial plastic surgery procedural volume. Laryngoscope 2020;130(3):632-6.
2. Bian X, Liu H, Sun J, Zhang X, Li N, Chen M. Efficacy of dexamethasone for reducing edema and ecchymosis after rhinoplasty: A systematic review and meta-analysis. Aesthetic Plast Surg 2020;44(5):1672-84.
3. Mirza AA, Alandejani TA, Al-Sayed AA. Piezosurgery versus conventional osteotomy in rhinoplasty: A systematic review and meta-analysis. Laryngoscope 2020;130(5):1158-65.
4. Ong AA, Farhood Z, Kyle AR, Patel KG. Interventions to decrease postoperative edema and ecchymosis after rhinoplasty: A systematic review of the literature. Plast Reconstr Surg 2016;137(5):1448-62.
5. Ping WD, Zhao QM, Sun HF, Lu HS, Li F. Role of tranexamic acid in nasal surgery: A systemic review and meta-analysis of randomized control trial. Medicine (Baltimore) 2019;98(16):e15202.
6. Gurlek A, Fariz A, Aydogan H, Ersoz-Ozturk A, Eren AT. Effects of different corticosteroids on edema and ecchymosis in open rhinoplasty. Aesthetic Plast Surg 2006;30(2):150-4.
7. Kargi E, Hoşnuter M, Babucçu O, Altunkaya H, Altinyazar C. Effect of steroids on edema, ecchymosis, and intraoperative bleeding in rhinoplasty. Ann Plast Surg 2003;51(6):570-4.
9. Tsikopoulos A, Tsikopoulos K, Doxani C, Vagdatli E, Meroni G, Skoulakis C, et al. Piezoelectric or conventional osteotomy in rhinoplasty? A systematic review and meta-analysis of clinical outcomes. ORL J Otorhinolaryngol Relat Spec 2020;82(4):216-34.
10. Gareis-Helferich E, de Decker W, Gross G, Dokter P, Geering H. [Closure of the conjunctiva using fibrinous tissue adhesives]. Klin Monbl Augenheilkd 1968;153(1):74-8, German.
12. Yu MS, Kim BH, Kang SH, Lim DJ. Combined use of crushed cartilage and fibrin sealant for radix augmentation in Asian rhinoplasty. Plast Reconstr Surg 2015;135(2):293e-300.
13. Pryor SG, Sykes J, Tollefson TT. Efficacy of fibrin sealant (human) (Evicel) in rhinoplasty: A prospective, randomized, single-blind trial of the use of fibrin sealant in lateral osteotomy. Arch Facial Plast Surg 2008;10(5):339-44.
14. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 2009;6(7):e1000097.
15. Yu MS, Jung MS, Kim BH, Kang SH, Lim DJ. Aerosolized fibrin sealant is effective for postoperative edema and ecchymosis in open rhinoplasty without osteotomy. J Oral Maxillofac Surg 2018;76(9):2000.e1-8.
16. Dayan SH, Bacos JT, Ho TV, Gandhi N, Gutierrez-Borst S. A pilot study evaluating the efficacy and safety of ARTISS human fibrin sealant in external rhinoplasty. Aesthetic Plast Surg 2018;42(2):590-7.
17. Chorney SR, Ryan JT. Fibrin sealant and parotidectomy wound complications in 100 patients. Eur Arch Otorhinolaryngol 2019;276(9):2621-4.
18. Dunn CJ, Goa KL. Fibrin sealant: A review of its use in surgery and endoscopy. Drugs 1999;58(5):863-86.
19. Lachachi F, Descottes B, Durand-Fontanier S, Sodji M, Pech de la Clause B, Valleix D. The value of fibrin sealant in thyroid surgery without drainage. Int Surg 2000;85(4):344-6.
20. Sircana G, Cauteruccio M, Oliva MS, Piccirillo N, Pesare E, Minutillo F, et al. Fibrin sealant reduces need for transfusions after hip hemiarthroplasty for femoral neck fractures. Injury 2020;51(Suppl 3):S23-7.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

 |
 |