Introduction
Perilymphatic fistulas (PLF) can be caused by various causes, including stapes surgery, head trauma, and inner ear erosion in chronic otitis media [1]. Symptoms of PLF are sensorineural hearing loss and dizziness.
Prognosis of hearing loss caused by PLF varies according to the time of occurrence and the type and severity of trauma. In the case of PLF due to barotrauma, the prognosis of hearing improvement is good if early surgical exploration is performed [2]. Dizziness caused by PLF may be a symptom of unilateral vestibular loss such as continuous whirling type vertigo and postural imbalance due to irreversible vestibular loss, or may also be symptom of positional dizziness. Atypical benign paroxysmal positional vertigo like positional nystagmus was found in the barotraumatic PLF [3].
Dizziness caused by PLF shows different prognosis according to the severity of vestibular loss and the characters of dizziness. If unilateral complete vestibular loss has occurred, vestibular rehabilitation can improve the vestibular symptoms.
In previous studies, dizziness caused by barotraumatic PLF often did not show unilateral vestibular loss [3], and vestibular symptoms improved when surgery was performed on a suspected PLF [4].
We experienced two cases of recurred dizziness a few years after PLF repair in the traumatic PLF on the oval window (OW).
Case
Case 1. Hearing loss and repeated vertigo after surgery for left chronic otitis media
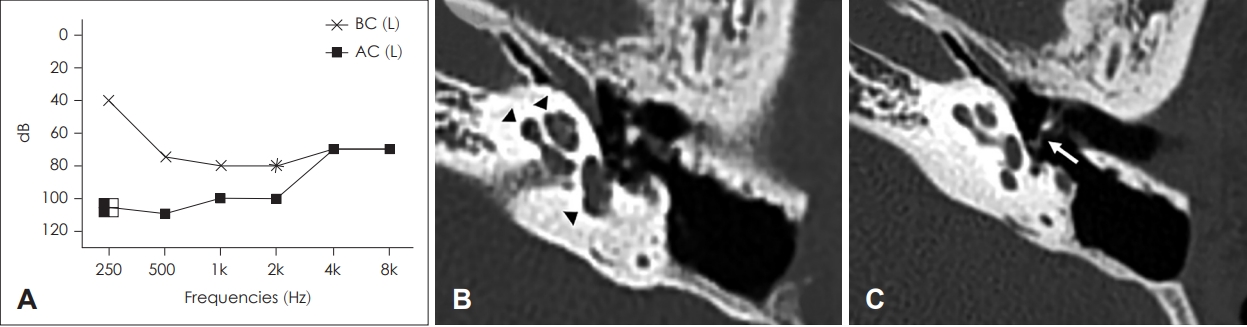
A 30-year-old man visited our clinic for left hearing loss and dizziness that has occurred immediately after canal wall up mastoidetomy with partial ossicular replacement prosthesis due to left chronic otitis media a year ago at another hospital. In the pure tone audiometry (PTA), the left ear had profound hearing loss (Fig. 1A). The vertiginous dizziness was caused by touching the ear and position change, which lasted less than 5 minutes. In videonystagmograph (VNG), spontaneous nystagmus and gaze evoked nystagmus were not observed. In the fistula test, the left beating horizontal nystagmus was induced by positive pressure in the left ear canal. In the caloric test, 64% of canal paresis was recorded on the left. The temporal bone (TB) CT showed no fracture line in the otic capsule, but a pneumolabyrinth was identified, suggesting a OW fistula (Fig. 1B). Under the suspicion of PLF around the stapes, and reoperation was performed. At the time of operation, the subluxation of the stapes footplate was found. The partial ossicular replacement prosthesis was removed, and the fistula was repaired by applying soft tissue and the fibrin glue around the stapes footplate. Any prothesis was not placed over the stapes head. Vestibular symptoms improved immediately after surgery. Hearing was not improved.
Three years after the operation, similar characters of dizziness recurred. The vertiginous dizziness was caused by touching the ear and position change, which lasted less than 5 minutes. The fistula test was positive. Recurrence of PLF was suspected due to a positive fistula test, and exploration was done under the local anesthesia. Definite PLF was not found, but there was a fibrous band between the stapes head and the tympanic membrane (Fig. 1C). The patient complained of subjective severe dizziness when touching the stapes during operation. Because it seemed that the dizziness was caused by the excessive movement of the stapes, the stapedectomy was done. After stapedectomy, occlusion of OW was performed with a soft tissue. On top of that, a silastic sheet was placed over the OW to block pressure transmission from the outside. Immediately after surgery, the patientвҖҷs dizziness disappears completely. He visited our clinic at 1 year postoperatively without any complaint about dizziness.
Case 2. Hearing loss and repeated vertigo after blunt head trauma due to traffic accident
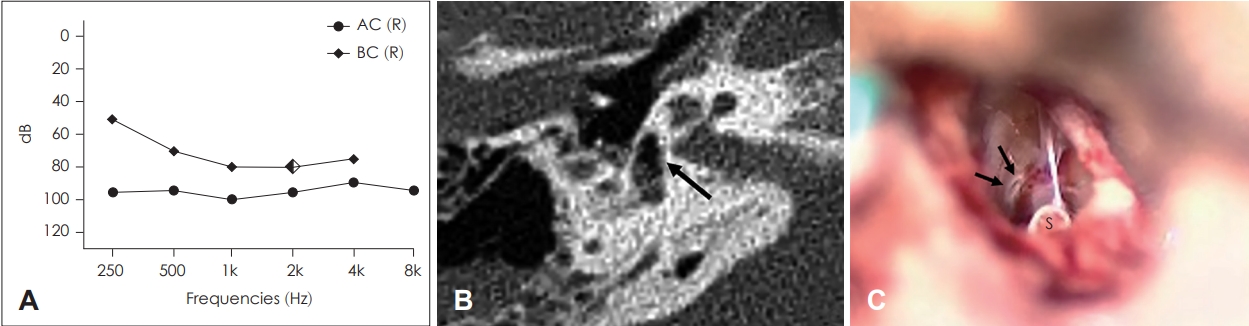
A 45-year-old female visited the hospital for a hearing loss and dizziness after a traffic accident 8 years ago. When she visited the clinic for the first time, she complained of lightheadedness, and the dizzy spell was worsened when the position changed, or when touching the ears or laughing loudly. PTA showed the right profound hearing loss (Fig. 2A). On TBCT after traffic accident, pneumolabyrinth in the vestibule was found (Fig. 2B). In the caloric test, right canal paresis (95% weaker) was recorded. Spontaneous nystagmus and gaze-evoked nystagmus were not observed in the VNG test and no significant nystagmus was observed in the positioning test, head shaking test. On fistula test, subjective dizziness was induced with upbeat nystagmus. Traumatic PLF was suspected and exploration was performed under local anesthesia. A fistula hole was identified in the OW with subluxation of the stapes (Fig. 2C). After removal of the incus, the fistula was repaired using soft tissue and cartilage. After surgery, the dizziness was completely improved. However, 8 years later, she revisited the clinic due to recurred dizziness. The symptom was induced when she put her finger in her ear or blow her nose. In the VNG, spontaneous nystagmus and gaze-induced nystagmus were not observed. In the fistula test, nystagmus was not observed, but subjective dizziness was complained. No abnormal findings were found on the TBCT. Exploration was performed under the suspicion of PLF under local anesthesia. In the surgical findings, the malleus handle were connected to the stapes head by the thick fibrous bands. Touching the stapes head during surgery induced subjective dizziness. Because it seemed that the dizziness was caused by the excessive movement of the stapes, the stapedectomy was done. After stapedectomy, we occluded the OW using soft tissue and cartilage. Thick silastic sheet (20/1000 inch) was placed over the OW. Dizziness disappeared completely immediately after surgery. Her last visit to our clinic was t 2 months after operation without any complaint about dizziness.
Discussion
We experienced two patients in similar findings who presented with positional dizziness and pressure induced dizziness after traumatic OW fistula. After fistular repair using soft tissue patch, the dizziness symptoms subsided, but the symptoms recurred a few years later. At revision surgery, even though actual fistula was not found, the stapes was connected with tympanic membrane by thick soft tissue band. When it was touched, the subjective dizzy spell was felt. After stapedectomy with soft tissue obliteration of OW, the dizzy spell subsided.
The two cases had several things in common. They were found to have OW fistula by iatrogenic injury (case 1) and blunt head trauma (case 2). Both cases had pneumovestibule after trauma on TBCT. At first operation, stapes subluxation (case 1) and definite fistular hole (case 2) was found. After repairing the fistula with soft tissue patching, the dizziness spell was subsided. At second operation after the dizzy symptoms recurred, no definite fistulas were not found, but thick fibrous band was connected between stapes head and tympanic membrane. They complained of dizziness when palpating the fibrous band or stapes head. After stapedectomy, the dizzy spells immediately subsided.
If the trauma causes dislocation and subluxation of the stapes, the PLF may occur at the OW, and pneumovestibule can be created. This causes sensorineural hearing loss and vestibular loss with whirling vertigo and unsteadiness because of severe damage of inner ear end organs [4]. Such hearing loss and vestibular loss is often irreversible, but subjective dizzy symptoms caused by unilateral vestibular loss tends to improve gradually by the vestibular compensation. However, if the PLF remains, postural dizziness or dizziness caused by middle ear pressure may persist.
In these cases, unilateral vestibular loss was initially proved in the caloric test, and the patient complained of subjective severe dizziness. These dizzy symptoms gradually improved as vestibular compensation proceeds over time. However, the patient was still complaining of positional dizziness if the fistula remains.
The mechanism of positional dizziness and pressure induced dizziness in PLF was not clear. Vestibular symptoms in chronic PLF have been assumed to be attributable to endolymphaic hydrops in the fistula ear [5]. On fistula test by canal pressure with a pneumatic otoscope (HennebertвҖҷs sign), nystagmus can be induced. In other animal study, artificial PLF could induce hydrops, rupture, and collapse of endolymphatic membrane in the inner ear. These pathologic change called вҖңfloating labyrinthвҖқ might be involved in prolonged subjective dizziness and nystagmus [6,7].
In our cases, iatrogenic and blunt trauma caused the disruption of annular ligament and subluxate the stapes. The stapes became floating, it can induce dizziness by stimulating the vestibuloocular reflex in the semicircular canal or the otolithic organs by pressure and positional change.
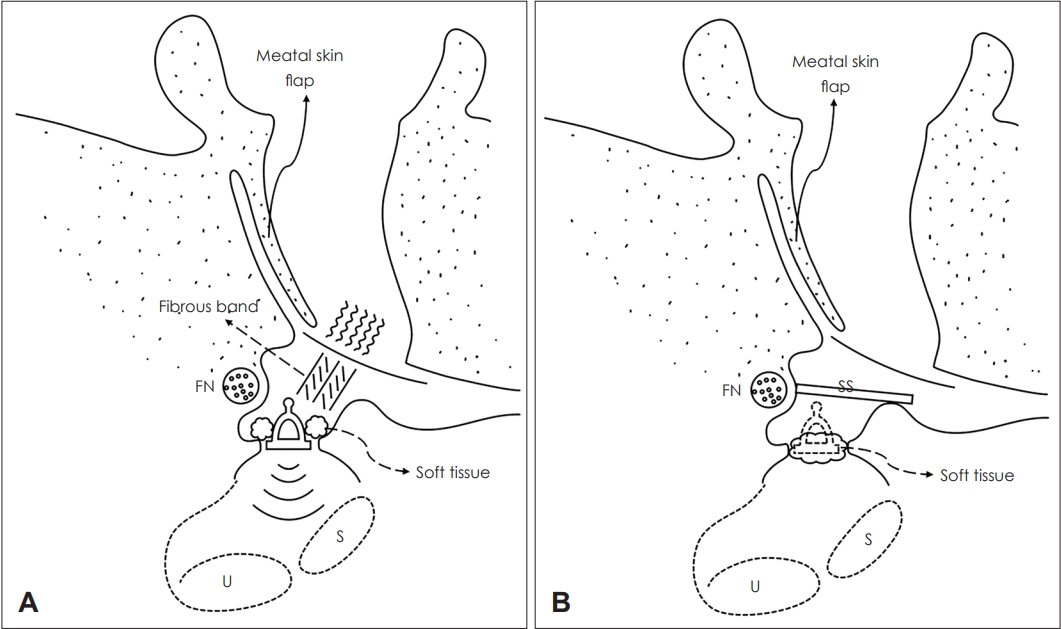
At the first operation, the stapes was not removed, and only the identified fistula was repaired with soft tissue, and the operation was completed. Dizziness improved immediately after the surgery. However, case 1 recurred after 1 year and 6 months, and case 2 after 8 years. In the second operation, there was a soft tissue connection by thick fibrous band between the stapes head and the tympanic membrane in both cases (Fig. 3A). The patient complained of severe dizziness when touching the fibrous band or the stapes. Therefore, it was confirmed that stapes movement caused dizziness, and this finding could explain the positive fistula test. Thus, after stapedectomy, the OW was occluded with soft tissue (Fig. 3B). Immediately after surgery, dizziness subsided completely in both patients.
The drawings showed the preoperative findings, and surgical procedure at revision operation (Fig. 3). My hypothesis for the mechanism of dizziness after OW fistula is the hypermobile stapes connected with inner ear endolymphatic membrane. Like HennebertвҖҷs sign, the stapes movement stimulated the vestibularocular reflex in the otolith organs. In normal inner ear, stapes movement is difficult to induce otolithic organs stimulation. This is because, in histological examination, the endolymphatic membrane of saccule and the stapes are separated from each other, and the perilymphatic fluid is present between them [8]. However, in MeniereвҖҷs disease, HennebertвҖҷs sign or Tullio phenomenon can occur. It means that endolymphatic membrane of the saccule contacts the stapes by endolymphatic hydrops, so the movement of the stapes by sound or pressure can stimulate the otolithic organs [9]. This causes the patient to complain of dizziness. Likewise, if the dislocation of stapes causing OW fistula changed the environment in the vestibule, such as hydrops, collapse, and rupture of endolymphatic membrane, or blood or inflammatory cells filling the vestibule, the movement of the stapes may stimulate the otolithic organs directed by interconnections between the stapes and the otolithic organs [6,10,11]. In addition, if the stapes mobility has been changed due to the dislocation of the stapes, the otolithic ogans may be more easily stimulated by stapes movement (floating stapes).
Interesting findings in these cases were nystagmus direction in fistula tests. Both cases showed positive fistula tests. In case 1, the nystagmus direction was horizontal with fast component directed to lesion side. However, in case 2. The nystagmus direction was upward. These meant that the stimulating organs seemed to be otolith organs rather than semicircular canals.
From these cases, we found two important findings. First was that OW fistula due to stapes subluxation could induce persistent chronic dizziness. Therefore, if the patients complaining of persistent dizziness is suspected of OW fistula, surgical exploration should be considered. Second, even after the OW fistula was healed spontaneously or surgically repaired, disabling dizziness could persist. The underlying mechanism for this might be interconnection between stapes and otolithic organs to cause the HennebertвҖҷs sign due to unstable floating stapes or the environmental change in the vestibule (floating labryrinth) or both.