Introduction
Primary thyroid lymphoma is a rare disease that accounts for less than 5% of all thyroid malignancies [1]. According to the current classification system, diffuse large B-cell lymphoma (DLBL) is the most common subtype [2]. One of the important features of thyroid lymphoma is that the tumor can grow rapidly over the course of only a few months, leading to airway obstruction [3]. In such cases, an emergency tracheostomy or early thyroidectomy is usually performed to secure the airway. Airway stenting is a type of interventional bronchoscopy that is widely used for the treatment of benign and malignant airway problems. Currently, a wide range of stent types (such as metal, silicone, self-expanding metal, and hybrid stents) are available for the management of different clinical conditions and their application has been shown to be effective in the treatment of malignant lesions, despite some side effects such as stent migration or malposition, granulation formation, infection, mucoid impaction [4].
Here, we report the recent case of a patient with primary thyroid DLBL who presented with airway compression but was not considered eligible for surgery. Therefore, a temporary tracheal silicone stent was inserted to allow time for chemotherapy to be administered. Along with a review of the literature, we report on the potential value of this approach in patients undergoing chemotherapy for primary thyroid DLBL.
Case
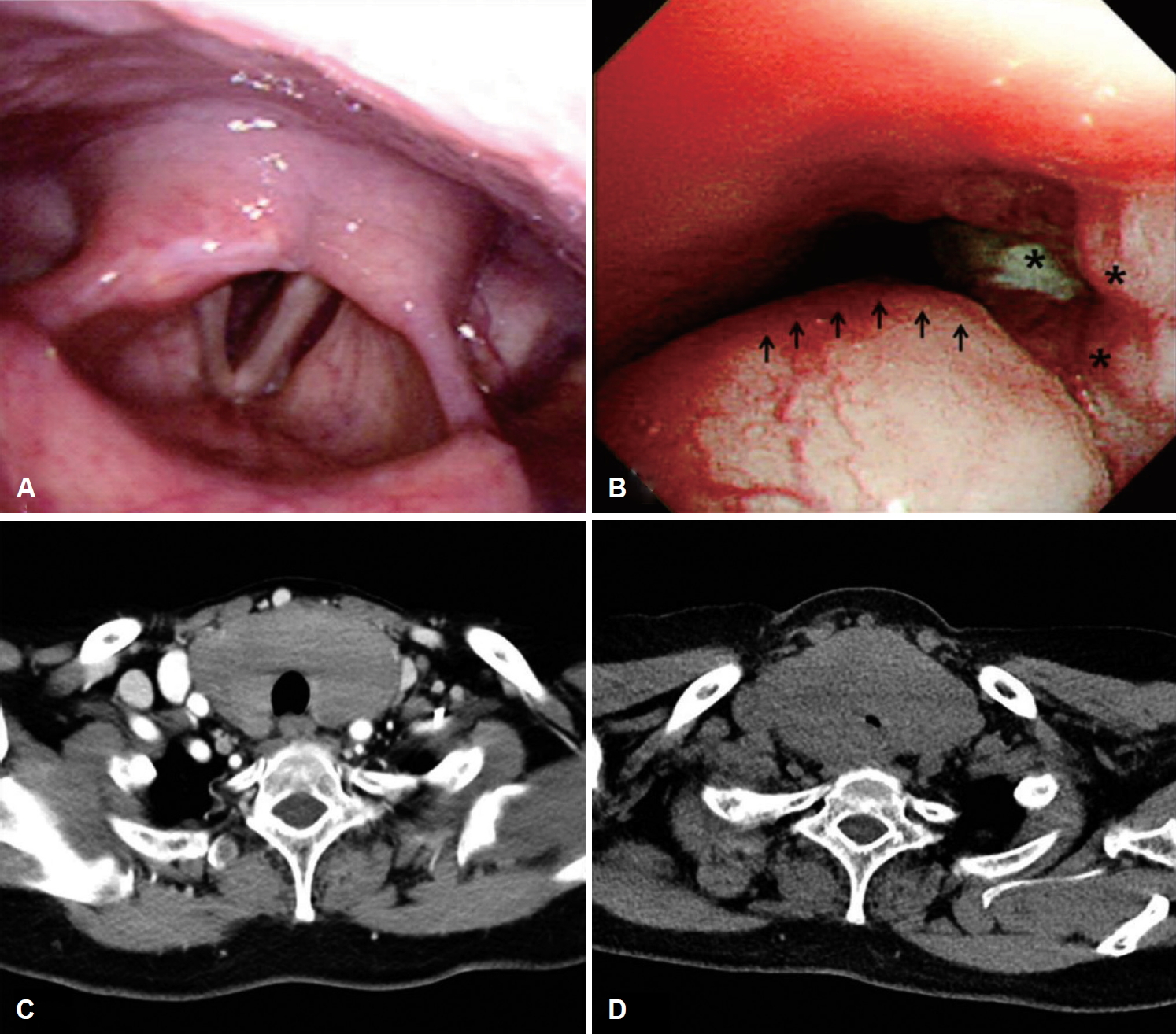
A 76-year-old woman presented with a 5 day history of dyspnea and was admitted to the pulmonology department of the Gyeongsang National University Hospital. Chest CT scanning showed an enlarged thyroid gland and narrowing of the upper airway, and the patient was referred to the otorhinolaryngology department. While taking the patientвҖҷs history, it was noted that she had been diagnosed with HashimotoвҖҷs thyroiditis 6 years previously and had been undergoing regular follow-up visits at the endocrinology department. An anterior neck mass had rapidly increased in size within the last 3 months. A diffusely enlarged thyroid gland was identified, but there were no palpable lymph nodes. Normal vocal cord movement was observed, and rigid laryngoscopic examination showed no lesions that may have accounted for the dyspnea (Fig. 1A).
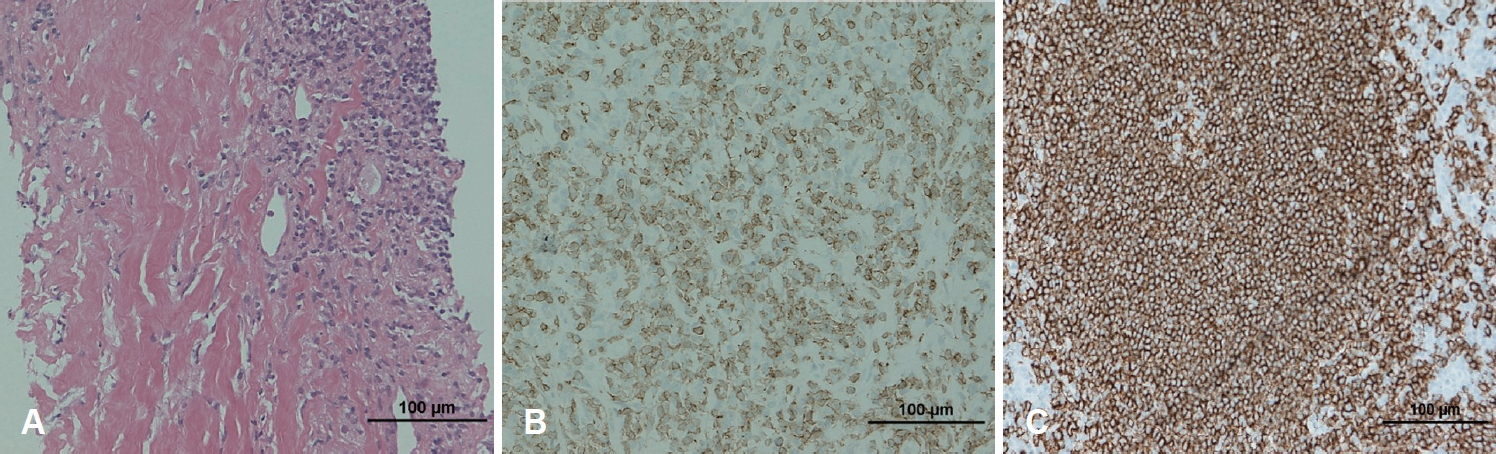
An additional bronchoscopy was performed to evaluate the upper airway, which showed that the endotracheal lumen was reduced by 70-80% due to external compression and localized ulcerating mucosal infiltration (Fig. 1B). During biopsy of the mucosal lesion, tracheal spasm resulted in hypoxia and subsequent cardiac arrest, requiring cardiopulmonary resuscitation to restore the patientвҖҷs spontaneous circulation. To obtain a more accurate radiological diagnosis, contrast-enhanced CT of the pharynx was performed, showing a notable increase in the size of the thyroid gland, tracheal deviation, and luminal narrowing when compared with chest CT scans obtained approximately 3 months earlier (Fig. 1C and D). A histological diagnosis was established by ultrasound-guided core needle biopsy, performed while the patient was intubated for airway maintenance. Hematoxylin and eosin staining showed diffusely infiltrated atypical lymphoid cells, which were shown to be strongly CD20-positive and weakly CD3-positive by immunohistochemical staining (Fig. 2). On the basis of these results, the patient was diagnosed with primary thyroid DLBL. Additional radiographic studies were performed to determine the stage of the disease, which showed involvement of the upper esophagus, bilateral cervical II, III, and IV lymph nodes, and bilateral supraclavicular lymph nodes, as well as the thyroid gland.
While surgery was considered to de-bulk the thyroid gland and secure the airway, the risks associated with a general anesthesia were deemed to be too high, considering the patientвҖҷs age, difficulty with intubation, and underlying diseases (such as hypertension, diabetes, asthma, atrial fibrillation, and history of cerebral infarction). Following a multidisciplinary team meeting, airway maintenance with endotracheal intubation during chemotherapy was agreed to be the preferred approach; however, the patient and her family insisted on stenting and an endotracheal silicone stent insertion was performed by a pulmonologist. Rigid bronchoscopy was performed under general anesthesia. After mechanical widening with serial rigid tubes, stent was placed in the stenotic trachea. Stent was a diameter of 12 mm and length of 50 mm considering normal diameter and narrowed vertical length of trachea.
The patientвҖҷs dyspnea resolved immediately after stent insertion, and chemotherapy with the rituximab, cyclophosphamide, hydroxydaunorubicin, vincristine, prednisolone (R-CHOP) regimen was initiated after 6 days. The plan was to remove the stent as soon as possible to avoid any associated complications; no events were noted up to 4 weeks after the start of chemotherapy. However, at 5 weeks, the patient complained of dyspnea, and pharyngeal CT was performed to identify the cause. This showed a significant decrease in the size of the thyroid gland and an absence of tracheal deviation and narrowing, but a soft tissue shadow was noted inside the stent and further exploration under suspension laryngoscopy was performed immediately (Fig. 3A). The narrowing of the stent lumen was found to be due to a sticky mucous plug, which was removed by repeated suction; no other findings were noted (Fig. 3B and C). The absence of tracheal compression was noted on both radiological and laryngoscopic investigation, and the stent was removed by a pulmonologist and the endotracheal lumen was widened enough to secure the airway (Fig. 3D).
While the patientвҖҷs dyspnea resolved after the removal of the stent, the patient developed neutropenia during preparation for the third cycle of chemotherapy and chemotherapy was discontinued. Subsequently, the patient developed pneumonia due to carbapenem-resistant Klebsiella pneumoniae infection. The patientвҖҷs general condition followed a repeated pattern of improvement and deterioration and she eventually died.
Discussion
Primary thyroid lymphoma is a rare disease that accounts for less than 5% of all thyroid malignancies and 1-2.5% of all lymphomas [1]. Under the revised European-American classification of lymphoid neoplasm and World Health Organization classification systems, it is now classified into DLBL, extra-nodal marginal zone B-cell lymphoma, and other rare subtypes [5]. Of these subtypes, DLBL is the most common variant [2]. As the thyroid gland lacks lymphoid tissues, most thyroid lymphomas arise from pre-existing chronic autoimmune thyroiditis [6]. The incidence of DLBL is approximately 67 times higher in patients with HashimotoвҖҷs thyroiditis [7].
Unlike most thyroid cancers, which are generally well-differentiated and slow-growing, anaplastic cancer and malignant lymphomas can grow rapidly and cause tracheal compression; emergent tracheostomy or early thyroidectomy may therefore be required to secure the airway [3,8]. The case presented here also showed rapid deterioration within 2-3 months. In terms of diagnosis, fine needle aspiration is often used to evaluate the thyroid mass, although the diagnostic accuracy is only approximately 60% due to histological similarities to HashimotoвҖҷs thyroiditis [9]. Therefore, in such cases, additional core needle biopsy or thyroidectomy may be required.
The treatment of primary thyroid lymphoma varies according to the subtype, histological findings, size, stage, and comorbidities. For DLBL, three cycles of R-CHOP is considered to be standard treatment; involved-field radiation therapy may be included in patients with advanced disease [10,11]. The current role of surgical management is primarily for the purpose of histological diagnosis and securing the airway, with a treatment goal being appropriate in only a limited number of cases. In the case presented here, surgical management was considered both for histological confirmation and to secure the airway. However, due to the patientвҖҷs age, pre-existing comorbidities, and severe tracheal narrowing, general anesthesia was considered to pose a high risk. In addition, the patient and her family wanted to avoid surgery if possible as the patient had experienced cardiac arrest during bronchoscopy. Following discussion by a multidisciplinary team, the decision was taken to proceed with chemotherapy under endotracheal intubation, although due to the patientвҖҷs preference for endotracheal stenting, this procedure was subsequently performed.
Tracheal stenting techniques have progressed in recent years, and a variety of stents are under development [4]. To date, few reports of stent insertion in patients with thyroid disease have appeared in the literature. In 2013, Shin, et al. [12] reported a successful case using a self-expandable metal stent and radiofrequency ablation therapy for a patient with multinodular thyroid goiter; Ding, et al. [13] reported excellent results using self-expanding metal stents for the treatment of mucosa-associated lymphoid tissue lymphoma. Madan, et al. [14] and Varadharajan, et al. [8] have also reported the usefulness of tracheal stenting in patients with anaplastic thyroid carcinoma. By contrast, Cho, et al. [15] noted serious complications after stent insertion in a patient with malignant lymphoma, and suggested that self-expandable metal stents should not be used in benign airway disease, with silicone stents being preferable in patients with benign or curable malignant airway disease.
Metal stents are usually net-shaped and are folded when inserted. They are self-expanding and resistant to external pressure, and show minimal displacement. However, the tumor can grow into the lumen of the stent and, therefore, removal can become difficult. By contrast, silicone stents are easy to adjust and remove, but are susceptible to external pressure and are easily displaced; therefore, various adverse events, such as stent displacement, granuloma formation, mucous plugging, bacterial growth, tumor ingrowth, and failure of adaptation, are known to occur [4]. In the current case, we intended to reduce the risk of complications by maintaining the stent for the shortest time possible. A silicone stent was selected due to concerns regarding tumor ingrowth and the fact that these stents are easy to handle and remove.
In the case presented here, chemotherapy was initiated 6 days after stent insertion and no complications were observed until two cycles of chemotherapy had been completed. However, the patient complained of dyspnea approximately 5 weeks after stent insertion. CT evaluation revealed a mucous plug in the lumen of the stent but also confirmed a remarkable decrease in the size of the thyroid lymphoma; the stent was subsequently removed successfully. Although there is the possibility that mucous stasis and bacterial colonization in the endotracheal stent contributed to the development of pneumonia, we consider that neutropenia as a complication of chemotherapy is likely to be the most probable cause. For such complications, Cho, et al. [15] have recommended surveillance examination with bronchoscopy 4-6 weeks after tracheal stent insertion regardless of symptoms and reported that the incidence of adverse events can be significantly reduced using this approach. Although our patient died as a result of developing pneumonia, this case has demonstrated the feasibility of carrying out chemotherapy after securing the airway through temporary stent insertion in patients with primary thyroid DLBL who are not eligible for surgery.
In patients with thyroid DLBL who present with airway compression but are not eligible for surgery, temporary endotracheal stent insertion can be an effective alternative that can secure the airway and enable continuous chemotherapy. In such cases, a stent can be maintained more safely through surveillance via bronchoscopy.